Specialist Advice — 13 minutes
Cigarette smoke makes it difficult to sleep and breathe

It is no secret that tobacco is harmful to a person’s health. However, its harmful effects do not stop at the cardiorespiratory system. Tobacco is also responsible for a variety of pathologies that lead to sleep disorders.

The sleep train is sometimes difficult to catch
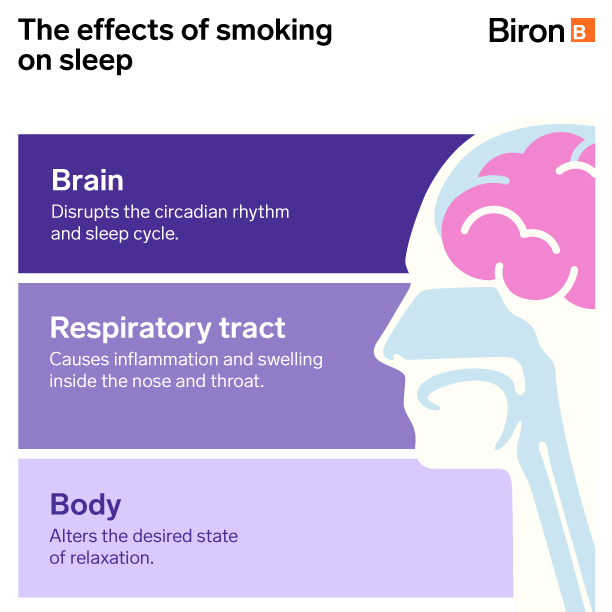
Similar to some drugs or doping products, nicotine is a powerful stimulant. One cigarette before bedtime can influence the body in the same way as a coffee and alter the state of relaxation sought. This can make it harder to get to sleep.
Tobacco also affects the airways, causing inflammation and even swelling inside the nose and throat. As a result, there is less room for air to circulate, which can lead to wheezing, snoring and poor overall sleep quality.
Smoking also disrupts the circadian rhythm and thus causes sleep fragmentation. It is also a cause of reduced NREM (deep) sleep. [1]
Tobacco and sleep apnea
Smoking can cause or amplify obstructive sleep apnea-hypopnea syndrome (OSAHS). Several studies have shown that people who smoke are more prone to sleep apnea than those who do not. Moreover, scientists have suggested that, in these situations, quitting smoking should be systematically considered in managing this health problem. [2] [3]
Furthermore, sleep-disordered breathing does not only affect smokers. Second-hand smoke is also harmful to those close to you, especially children. [4]
Smoking cessation and insomnia
Because nicotine is a powerful stimulant, its deprivation causes a feeling of fatigue that can last two to three weeks. The brain also has to deal with the different demands of daily life without its usual pick-me-up. Therefore, a period of adaptation is completely normal.
At the same time, the sleep rhythm is changed. Nightmares, insomnia and even night sweats can occur during the first three or four weeks of withdrawal. Symptoms associated with nicotine withdrawal also favour a further disruption of the sleep architecture. [5]
Other unpleasant signs of detoxification may appear during the day. However, many drug and non-drug treatments exist to help a person get through this period more calmly. Medical advice is often preferable to benefit from proper support during this process and increase the chances of success.
Detoxing to avoid COPD
Smoking is recognized as the leading cause of chronic obstructive pulmonary disease (COPD). According to Health Canada, [6] the risk of dying from COPD increases with the number of cigarettes smoked daily and the number of years of addiction.
The multiple chemicals contained in cigarette smoke irritate the bronchial tubes and lung tissue. They also destroy the cilia that help filter and clean the lungs. This process eventually leads to breathing difficulties that only get worse with time.
What is COPD?
COPD includes two conditions, which occur simultaneously most of the time:
- Chronic bronchitis: Permanent inflammation of the bronchial tubes and the production of mucus (secretions) that cause constant coughing, breathing difficulties and shortness of breath
- Emphysema: Degenerative disease due to the progressive destruction of lung tissue that reduces the amount of oxygen available in the body. This condition causes persistent shortness of breath and increasing fatigue. [7]
Overlap syndrome
COPD and obstructive sleep apnea respectively affect 20% and 10% of the population over 40 years old. The combination of these two health conditions is called "overlap syndrome". Studies suggest that smoking plays a determining role in the appearance of symptoms.
This pathology leads to a varying degree of oxygen desaturation (decrease of oxygen level in the blood). This increases the risk of developing respiratory failure or pulmonary hypertension. [8]
Patients with overlap syndrome usually need to be treated at night with a combination of a continuous positive airway pressure device (CPAP) and oxygen. Non-invasive ventilation (NIV) can also be used. This involves the use of a ventilatory device connected to a mask that the person puts on at night and that provides the necessary breathing support, mainly when apneas occur. This system, available only by prescription, is the initial treatment for regulating apneas and must generally be used over a long period of time, even continuously in order to be effective. [9]
Immediate benefits after quitting smoking
To limit the risk of COPD or other cardiorespiratory illnesses and improve sleep quality, smoking cessation is an excellent option to consider.
 What’s more, you do not have to wait 10 years to measure the benefits:
What’s more, you do not have to wait 10 years to measure the benefits:
- After 20 minutes, blood pressure and the heart rate decrease. Hand and foot temperatures return to normal.
- After 8 hours, the level of carbon monoxide in the blood decreases. The amount of oxygen in the blood increases to a normal level.
- After 24 to 48 hours, the risk of a heart attack drops, taste and smell improve.
- After 2 to 3 months, blood circulation improves and lung function increases by up to 30%.
- After 9 months, coughing, sinus congestion, fatigue and shortness of breath decrease. The lungs become clearer and more resistant to infection.
In the long term, the risks associated with serious illnesses decrease, sometimes to a significant degree:
- After 4 to 5 years, the risk of a stroke (cerebrovascular accident) is the same as in a non-smoker. [10]
- After 10 to 15 years, the risk of developing lung cancer is reduced by half. [11]
Is willpower enough to deal with the challenges of withdrawal?
According to most specialized sites, the chances of success using willpower alone are about 1% or 2%. Nicotine addiction is actually comparable to cocaine or heroin addiction. [12] Under these conditions, it seems illusory to hope to overcome one’s addiction without support.
Whether you opt for transdermal nicotine patches, medications or behavioural therapies, there is no shortage of ways to increase your success rate. To achieve the best results, it is advisable to consult your doctor or pharmacist, or even to search specialized sites or call a line dedicated to the fight against smoking.
For professional support, we’re here for you.
We provide services that can help your doctor diagnose sleep disorders and determine the appropriate treatment.
- Sleep Care services
- Online Screening
- Free remote consultation with our respiratory therapist
- Sleep hygiene program
You have question about an equipment? Chat online with our respiratory therapist.
Sources12
- D. W. Wetter and T. B. Young, “The relation between cigarette smoking and sleep disturbance,” Prev Med, vol. 23, no 3, May 1994, p. 328-334. https://pubmed.ncbi.nlm.nih.gov/8078854/ (source consulted November 1, 2021).
- S. Maalej, O. Neffati and H. Souir, “Tabagisme au cours d’apnées hypopnées obstructives du sommeil : prévalence et influence,” Médecine du sommeil, vol. 13, no 1, March 2016, p. 41. https://www.researchgate.net/publication/297611489_Tabagisme_au_cours_du_syndrome_d'apnees_hypopnees_obstructives_du_sommeil_prevalence_et_influence (source consulted November 1, 2021).
- L. Boussoffara et al., “Tabagisme et sévérité du syndrome d’apnées hypopnées obstructives du sommeil,” Revue des maladies respiratoires, vol. 30, no 1, January 2013, p. 38-43. https://www.lissa.fr/rep/articles/23318188 (source consulted November 1, 2021).
- S. M. Jara et al., “The association between secondhand smoke and sleep-disordered breathing in children: A systematic review,” The Laryngoscope, July 31, 2014. https://onlinelibrary.wiley.com/doi/10.1002/lary.24833 (source consulted November 1, 2021).
- Centers for Disease Control and Prevention, “7 Common Withdrawal Symptoms and What You Can Do About Them,” June 18, 2021. https://www.cdc.gov/tobacco/campaign/tips/quit-smoking/7-common-withdrawal-symptoms/index.html (source consulted November 1, 2021).
- Health Canada, “Smoking and Chronic Obstructive Pulmonary Disease,” September 22, 2011. https://www.canada.ca/en/health-canada/services/health-concerns/tobacco/legislation/tobacco-product-labelling/smoking-chronic-obstructive-pulmonary-disease.html (source consulted November 1, 2021).
- Association pulmonaire du Québec, “COPD, emphysema and bronchitis.” https://poumonquebec.ca/en/maladies/copd/ (source consulted November 1, 2021).
- E. Weitzenblum et al., “Overlap Syndrome: Obstructive Sleep Apnea in Patients with Chronic Obstructive Pulmonary Disease,” Proceedings of the American Thoracic Society, vol. 5, no 2, September 6, 2007. https://www.atsjournals.org/doi/full/10.1513/pats.200706-077MG (source consulted November 1, 2021).
- C. Massebiau et al., “Ventilation non invasive (VNI) chez l’adulte,” Hôpitaux universitaires Genève, June 18, 2020. https://www.hug.ch/procedures-de-soins/ventilation-non-invasive-vni-chez-adulte (source consulted November 1, 2021).
- Organisation mondiale de la santé, “Le tabac et les accidents vasculaires cérébraux,” 2016. https://apps.who.int/iris/bitstream/handle/10665/332583/WHO-NMH-PND-CIC-TKS-16.1-fre.pdf?sequence=5&isAllowed=y (source consulted November 1, 2021).
- U.S. Department of Health and Human Services, “Smoking Cessation: A Report of the Surgeon General,” 2020. https://www.hhs.gov/sites/default/files/2020-cessation-sgr-full-report.pdf (source consulted November 1, 2021).
- Tobacco-Free Quebec, “Your Mental Roadblocks.” https://tobaccofreequebec.ca/iquitnow/still-hesitating/mental-roadblocks (source consulted November 1, 2021).











